Aged Care in Australia 2007 – 2008
The Minister for Ageing, Justine Elliot, commented in her media release in November, 2008:
- During 2007-08, the Aged Care Standards and Accreditation Agency conducted 5,244 visits to aged-care homes. 3,105 visits were unannounced.
- In this same period the Department of Health and Ageing undertook 3,127 visits to aged-care homes, of which 1,145 were unannounced.
- The Accreditation Agency identified 46 homes (1.6 per cent) that had some non-compliance in relation to the 44 accreditation standard outcomes.
--- The Minister made further comment in her media release on 26 November, 2008:
"The data speaks for itself. It shows the vast majority of nursing homes are providing a world class service, but there is a small group - 46 nursing homes - that had failed to meet 44 accreditation standard outcomes under the Aged Care Act."
When 46 failed homes really means 199
The Minister also states in the Report on the Operation of the Aged Care Act 1997 - 1 July 2007 to 30 June 2008:
"only 1.6 per cent of homes (46 homes) were identified as having some non-compliance in respect to the 44 Accreditation Standard expected outcomes"
Aged Care Crisis records indicated that at least 108 (3.8%) of aged-care homes did so. We wrote to the Minister prior to publishing our findings along with supporting data, seeking clarification of the discrepencies, together with the data source available to us at the time.
This was based on information that we were able to access published on-line (at various stages throughout the year) by the Agency and the Department. Based on the limited information that is publicly available, the data may not be contemporaneous and these findings were tentative at the time.
Update - 16 Dec 2008: After being approached by media, The Minister stated that 199 (7%) of aged-care homes were identified as having some non-compliance over the year.
Update - 16 Jan 2009: A reply from the Minister's office, along with an explanation of the number of non-compliant nursing homes figures from 46 Vs. 199:
"The Report correctly indicates that, on 30 June 2008, 46 aged care facilities were operating with some level of non-compliance with the Accreditation Standards. The Report does not include instances of non-compliance in cases where the non-compliance was rectified prior to 30 June 2008."
* "I appreciate that this may not be clear to readers and we will review how the figure is represented in future reports."
* Groundhog day: Fast forward to 2016, and the renamed Quality Agency seem to have adopted the same style of reporting.
Summary of our analysis
1. | Our analysis of the 108 aged-care homes within our records indicates that government and community-based not-for-profit providers had, proportionally, more than twice the number of homes not meeting required standards compared with charitable and religious providers. The data indicates that this is because many more of their homes are located in rural and remote parts of the country, distant from resources. Our conclusion is that this group requires more support than it is currently receiving. |
2. | Even though 97 percent of private-for-profit operated aged-care homes which did not meet the required standards were centrally located, they too had double the incidence of failed standards. |
3. | To eliminate the bias introduced by the large number of remote aged-care homes operated by some not-for-profit groups, and to make a more valid comparison with the performance of the private-for-profit operators, we did a further analysis excluding all peripherally located facilities. The difference in the performance of the different not-for-profit groups now disappeared. The private-for-profit aged-care homes now had twice the number of homes failing one or more standard than the government operators, three times that of any of the not-for-profit operators and almost 4 times the religious based subgroup - the largest of these. We did not have the information needed to evaluate all of the factors that might have contributed to these findings. In particular we had insufficient information about the size and structure of owners, providers and management units to make any assessment of these factors. We express our concern that the higher proportion of private-for-profit operators within the failing facilities may have been because both financial and human resources are being diverted from the care of the frail, older people to the business of generating profits and capital expenditure compared to the ongoing costs of providing quality care and ensuring there is adequate and experienced staff to look after residents. |
4. | These findings fuel our frustration at the lack of transparency within the aged-care sector – frustration which is shared by other consumer groups. The Rudd government has pledged to achieve greater transparency across all areas of government. Yet, there is too little evidence of this within the aged-care sector – an area where the vulnerability of people is extremely high and the need for protection paramount. We call on the Minister, as well as the various departments and oversight bodies, to introduce far greater transparency in reporting and to cooperate fully with those prepared to devote their time and their skills to finding ways to improve the care received by frail, older people. |
Introduction
The Aged Care Act 1997 heralded a major change in the provision of aged care in Australia. Care of the aged and infirm was turned into a commodity which was able to be traded in the market place. It is astounding that, ten years later, the Department of Health and Ageing has provided no detailed evaluation of this major development which has affected so many frail, older Australians. A lack of full transparency by all authorities responsible for monitoring this process has prevented other interested parties from doing so.
The Aged Care Crisis Team now calls for a complete, open review of the Aged Care Act 1997, and asks for a thorough examination and analysis of all aspects of aged care. The sector, and those it serves, deserves no less.
The Aged Care Crisis Team has gathered information from various sources during the last few years but it is necessarily incomplete. We were stimulated to closely examine some of this data as documents in our possession indicated that more than twice the number of facilities failed full accreditation than the 46 claimed by the Minister for Ageing in her media releases.Based on the limited information that is publicly available, the data may not be contemporaneous and these findings are tentative.
What is clear is that useful information, on which public policy and democratic debate should be based, is not fully available to public scrutiny. Particularly worrying is that a system based on market place dynamics conceals the information which citizens require to make effective decision making. Frail citizens and their families are therefore unable to make rational choices when selecting a nursing home. As well, hospital and community social workers are unable to appropriately advise them.
Many families contact the Aged Care Crisis Team about failures in care. We suspect that the incidence of failure is far higher than that detected and published by the Aged Care Standards and Accreditation Agency and the Department of Health and Ageing. At present we have no way of confirming this.
We stress that there are two issues here - the validity and effectiveness of the accreditation process and the actual accreditation findings. Our present analysis examines the assessment findings but does not address their validity or effectiveness.
The data
The Aged Care Crisis Team had collected reports on 108 aged-care homes in which one or more of the 44 accreditation standards were found wanting and/or sanctions were imposed during the period when the Minister reported just 46.
A list of the 108 aged-care homes in this analysis is provided further down this page. The analysis appears to be representative and we believe give an indication of trends within the sector.
We have included those aged-care homes where our records show that they failed non-compliance between 1st July 2007 and 30 June 2008 and/or were sanctioned during this period indicating that failures persisted. Earlier failures were excluded unless sanctions were imposed during the study period. We note that some nursing homes and hostels, particularly in rural and remote areas, although having similar names, are separately registered and assessed. They appear to be co-located but separate. We have treated them as such.
We have analysed this information looking for pointers to what is happening. Further studies based on complete data are urgently needed to confirm the validity and the independent impact of the different factors examined.
Analysis
Distribution of aged-care homes
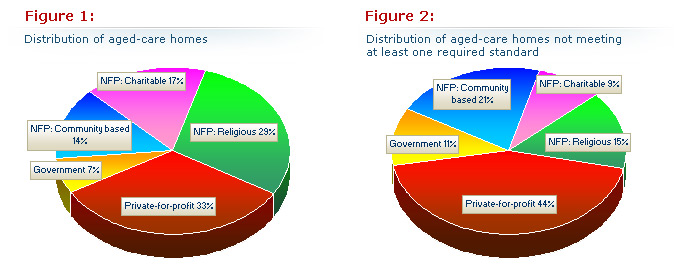
As of June 30, there were 2,838 Commonwealth-funded aged-care homes in Australia. The proportion of aged-care homes, expressed as a percentage figure, is shown in Figure 1 (below).
The Minister's report and other data available to us indicate that not-for-profit groups operated 1,698 (59.7%) homes. Of these 821 (29%) were run by religious groups, 481 (17%) by charities, and 396 (14%) by community based groups.
Governments operated 198 (7%) and private-for-profit operators 942 (33.7%). This categorisation is based on a document which we believe originated within the Department of Health and Ageing.
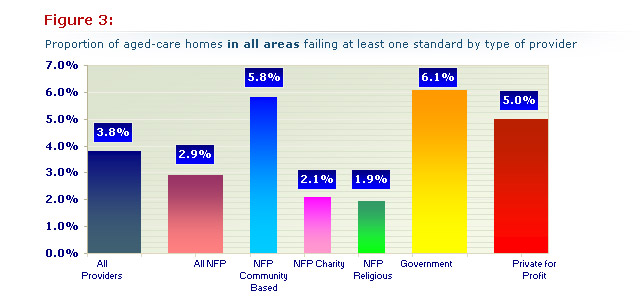
Distribution of aged-care homes not meeting at least one required standard
The distribution changes when the 108facilities that failed at least one accreditation standard are examined. Private-for-profit 47 (44%), government 12 (11%) and community-based not-for-profit 23 (21%) each had an increased proportion of the failed homes. In contrast, charitable 10 (9%) and religious not- for-profit 16 (15%) had a much smaller proportion. They accounted for only a quarter of the failed aged-care homes even though they operate nearly half of all aged-care homes (Figure 2)
In Figure 1 (left), the proportion of all 2,838 Australian nursing homes by approved provider type (left) compared with Figure 2 (right) the proportion of 108 Australian nursing homes that had some non-compliance by approved provider type. Note that the charitable and religious groups have halved the proportion of the failed homes whereas the other three have increased indicating that the problem homes lie mainly here.
Incidence of failures
Using the figures above it was possible to calculate the proportion of aged-care homes failing an accreditation standard in each group and then compare the rate of accreditation failures for each to give an indication of performance in Figure 3 (below):
The best performers were the charitable and religious not-for profit sub-groups. They had less than half the rate of private-for-profit providers and almost one third the rate of government-run and community-based not-for-profit aged-care homes.
A more accurate, but still not fully comparable comparison between the private-for-profit and not-for-profit providers, is given by comparing the for-profit private providers with the charitable and religious not-for-profit groups only. The latter operate fewer peripherally located failing services (23%) than the government and community based groups (63%). Only 4% of the failing private-for-profit providers are peripheral with 96% central. When compared with the charity and religious groups, the private-for-profit operators had more than double the proportion of failing homes - see Figure 3 (above).
Number of standards failed
The average number of the 44 accreditation standards failed did not differ much between the various groups. The charitable and not-for-profit religious organisations had fewer but the numbers were insufficient to draw any firm conclusions.
Government operated aged-care homes averaged 10.7 failures, community-based not-for-profit 9.7, not-for-profit charitable 6.0, not-for-profit religious 6.9 and private-for-profit 9.0.
The impact of distance
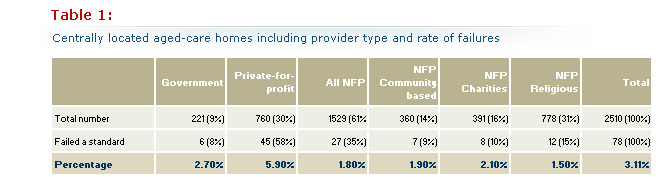
Isolation by distance from major centres and medical services is likely to be associated with limited management resources, fewer trained staff, and less oversight by parent organisations and other bodies. They are therefore at a disadvantage.
The differences in distribution between peripheral groups of aged-care homes in outer regional, remote and very remote areas - when contrasted with central groups comprising inner regional and major city areas - is striking. These readily account for the differences seen between the government and community-based groups on the one hand and the charitable and religious groups on the other. Both are more likely to serve those in need in their own localities.
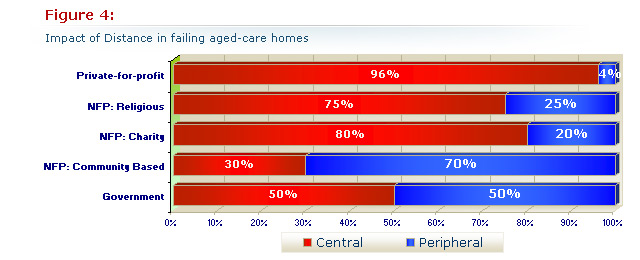
Figure 4 (above), shows the proportion of the 108 nursing homes failing at least one standard owned by each sort of provider group in central and peripheral areas.
The impact of private-for-profit control of aged care
As a more peripheral location clearly was associated with failures in standards we re-examined the data after excluding all of the peripheral facilities. To get the information we needed we used a different data source with 2,937 (107 more facilities) listed in Australia. This was not a significant difference, We excluded 427 peripherally located facilities leaving 2,510 more central ones for analysis. When we excluded the 30 peripherally located aged-care homes that had failed a standard we were left with 78 that were centrally located. The distribution of both groups by provider group as well as the rate of failure is shown in Table 1 (below):
The percentages of failed aged-care homes graphed in Figure 5 (below) can be compared with Figure 3. The bias created by distribution has disappeared so that government and not-for-profit subgroups now perform similarly.
The private-for-profit sector stands out with more than twice the incidence when compared with government, over three times when compared with all not for profits and almost four times when compared with the largest not-for-profit group, the religious providers.
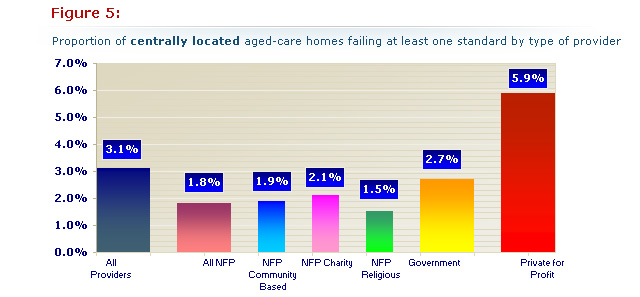
Figure 5 (above): Note that the change in distribution in each group differs from our first analysis (Figure 3), in that the private-for-profit sector has more than double the rate of failing aged-care homes than all the other groups which now perform comparably.
Discussion
The data indicates that peripherally located nursing homes are disadvantaged and need greater integration and support.
The size of the provider organisation and the managerial resources and experience it can bring to its operations are clearly important. Our impression is that providers with fewer aged-care homes are both more likely to fail accreditation standards and more likely to have more than one home fail. The complexity of the managerial and corporate structures in both the private-for-profit and the not-for-profit sectors coupled with the lack of transparency in these matters would make any attempt to analyse or draw firm conclusions in this regard from our limited data prone to error. We have not attempted to do so.
In looking at factors other than the provider type that might influence the results and produce the other changes, we feel that the imbalance in our outcomes might be partly biased in that the not-for-profit religious and charity subgroups have fewer small operators who also seem to be more at risk. It is unlikely that this would account for all the difference. If this is so, then this has policy implications.
Private-for-profit operators generally serve the more affluent sections of the community in centrally located areas. We feel that they should not lack for resources or community support. As indicated earlier we did not have the information needed to evaluate the impact of these and other factors. The market makes claims to greater efficiency but if so then these results suggest that this does not extend to improving accreditation outcomes. It is clearly essential that these results be validated by a much larger study including all the data from the last 3-4 years and including an assessment of corporate and management size and structure.
We are deeply concerned that these findings are a consequence of the diversion of financial and human resources from the care of residents to the care of profits. The industry's own figures lend support to our concerns. The December 2008 Aged Care Association of Australia's (ACAA) submission (pages 6-7, Graph 2-Graph 3) to the Australian Senate Finance and Public Administration Committee reveals that the profit margin of for profit nursing home operators (16%) is double that of not-for-profit operators (8%). It also reveals that private-for-profit providers make three times the net profit from each bed ($3,000 vs $1,000). Our results suggest that this has consequences.
We are also concerned that this may be a red flag pointing to a pervasive change in ethos and a consequent malaise in the sector; a malaise, pointed to by the number of nurse whistle blowers, falling staff levels, rising community concern and the succession of scandals since 2000. If these findings are replicated in a more thorough study then this would be a serious indictment of the policies embarked on in 1997.
In the USA, where far more detailed information is publicly available, most studies comparing not-for-profit and privately-operated corporate owned aged-care nursing homes have, over the years, found that the latter have about 3 times as many problems. It is interesting that our findings are similar. We suspect that a more comprehensive study would confirm this as well as identifying the impact of other factors.
Conclusions
The admittedly limited data available to us indicates that government and community-based not-for -profit operators have more than double the incidence of aged-care homes failing at least one accreditation standard when compared with other not-for-profit providers. This is readily accounted for by the number of facilities located in more remote areas of Australia.
Private-for-profit operators which operate almost entirely in central areas have a similarly higher incidence of aged-care homes not meeting required standards. It has not been possible to evaluate all of the factors which might impact on this. It concerns us that the difference may be because human and financial resources are being diverted from the care of residents to the business of extracting profits from the sector.
Further investigations to confirm the validity of these findings and to evaluate the impact of the other factors at work are required. We urge the government to make data publicly available so that academics and members of the community can bring their many skills to an evaluation of the issues, and their talents to addressing the way ahead. The baby-boomer aged-care bulge is upon us and to do otherwise would be irresponsible. We cannot afford to squander our country's talents.
Additional comments and information
The following sliders contain additional information and comments about the data and the accreditation process:
Comments on the data
We are somewhat confused by the varying use of terminology within the Minister's media releases and announcements. We assume that, although the Minister refers to 46 homes that failed to meet required standards in her media release of 25 November 2008 [Release of annual report – Operation of Aged Care Act 2007-2008], she was actually referring to both nursing homes and hostels – 1.6 percent of all aged-care homes.
Comments on the lack of transparency
An unfulfilled promise: The Rudd government has promised greater transparency in all spheres of government but there is little evidence of this within the aged-care sector. We believe that the issue of increased transparency was largely ignored in the November 2008 revision of the Aged Care Act 1997. It is our view that both the Accreditation Agency and the DHA should collect and collate all information relating to the provision of aged care and ensure that it is readily accessible to all. We also believe that there must be far more involvement from communities and much more community input into all aspects of aged care – including the accreditation process.
Accreditation and transparency: The current limited system of late release and early removal of adverse reports from the Aged Care Standards and Accreditation Agency website is unsatisfactory. Consumers are entitled to disclosure of all past, as well as present, reports. Information needs to be presented in a digestible format. As already stated, frail older people are one of the most vulnerable groups in society and their protection should outweigh all other considerations.
In order to achieve this protection, community members must be able to see what the company or provider is capable of when no one is watching - not just when they have been given time to prepare for an inspection and not simply after providing a response to an adverse finding in order to stay in business.
Minister's media release
Release of annual report – Operation of Aged Care Act 2007-2008
MEDIA RELEASE: 25 November 2008
The Minister for Ageing, Mrs Justine Elliot today released the annual report into the Report into the Operation of the Aged Care Act 2007-2008.
It showed 300,000 Australians received care through the record support for the aged and community care sector provided by the Rudd Labor Government.
Currently, there are some 2.8 million Australians – about 13 per cent of the population – aged 65 and over. This number is expected to triple in 40 years.
"Australia has the world's second longest life expectancy and the Australian Government is responding to the challenge of an ageing population," Mrs Elliot said.
"Over the next four years, the Australian Government will invest more than $41.6 billion into aged and community care. We will provide on average $41,500 a year a resident in subsidies. No Government has invested more into this area than the Rudd Government.
"We want to ensure the long-term viability of the aged sector, but also ensure that there are quality and accreditation standards to protect vulnerable members of our society," Mrs Elliot said.
In 2007-2008, more than 300,000 people received a form of aged and community and the Federal Government provided $8.3 billion for ageing and aged care in Australia.
As of June 30, there were 2,830 nursing homes and hostels in Australia; 174,669 residential places; 46,475 community care places and 1,963 transition care places.
The report covers July 1, 2007 to June 30, 2008, including the final four months of the previous Government.
Section 63-2 of the Aged Care Act requires the Minister for Ageing to present a report on the operation of the Act for 2007-2008 before November 30.
Key facts: Report on the Operation of the Aged Care Act
Aged and Community Care – 2007-2008
- 208,079 people received permanent residential aged care;
- 39,443 people received short-term respite care in aged care homes; of whom 18,415 were later admitted to permanent care;
- 61,739 received care at home through a community care or flexible care package;
- 10,351 received transition care following a hospital stay;
- 53,074 admissions to residential respite care, and care recipients used an estimated 1.18 million resident days;
- A total of 10,874 new aged care places were allocated nationally during 2007-2008;
- About 831,500 individuals received a form of Home and Community Care (HACC) service – with some receiving more than one service; and
- A total of 188,967 Aged Care Assessments were completed in 2006-2007, compared with 179,354 for 2005-2006.
Aged and community care providers
- As of June 30, there were 2,830 nursing homes and hostels in Australia;
- In 2007-2008, the nursing home and hostel comprised – religious, charity and community based (59.7 per cent); for-profit/commercial (33.3 per cent) and State and local governments (7 per cent);
- In 2007-2008, the community care sector comprised – religious, charity and community based (83.6 per cent); State and local governments (11.7 per cent) and for-profit (4.7 per cent).
Expenditure – 2007-2008
- Overall Federal government expenditure for ageing and aged care during 2007-2008 totalled $8.3 billion compared with $7.7 billion in 2006-2007 – an increase of 7.8 per cent in 2006-2007;
- $6 billion was spent on residential aged care;
- $448 million for Community Care Packages – an increase of 10.6 per cent over 2006-2007;
- $335 million for flexible care programs, including Extended Aged Care at Home (EACH) and EACH – Dementia packages, Multi-purpose Services and Transition Care;
- Average accommodation bond charged to a new resident by providers was $188,798 in 2007-2008;
- the average holding per approved provider was $6.5 million and the 10 largest bond holders held about 19 per cent ($1.2 billion) of all accommodation bond monies; and
- Thirty-five per cent (6,098) of the 17,132 Resident Classification Scale reviews resulted in re-classifications – meaning the funding claims made by providers accurately matched the level of care for people living in nursing homes.
Expenditure – 2008-2009
- Over the next four years to 2011-2012, funding for aged and community care will reach record levels of $41.6 billion.
- Funding in 2008-2009 for community care services will total $2.2 billion – an increase of $260 million over 2007-2008;
- For 2008-2009 alone, there will be an increase of 10.4 per cent in funding for aged and community care;
- The new Aged Care Funding Instrument (ACFI) that commenced on March 20 with bipartisan support will see more than $1.13 billion in additional funding to the residential care sector over the first four years of its use;
- An increase in the Conditional Adjustment Payment (CAP) in the 2008 budget will see an increase of more than $407 million over the four years to 2011-12 flow to the sector – bringing the total CAP funding for aged care to $2 billion;
- Allocation of $150 million in Zero Real Interest Loans to create 1,455 nursing home beds and community care packages for older Australians in areas of high need – with 375 and 154 places in Western Australia and Tasmania, respectively; and
- Allocation of 228 new transition care places under its $293.2 million plan – to help older Australians recover from a hospital stay and return to their own homes. The 228 places are expected to benefit up to 1,710 older Australians – in a full year. Each funded place will be used by up to eight different older Australians a year.
Construction/upgrading work
- $1.45 billion worth of new building, refurbishment and upgrading work was completed to nursing homes during 2007-2008 – involving about 13.4 per cent of all homes;
- $1.93 billion of construction work was in progress as at June 30, 2008 – involving 9.8 per cent of all homes; and
- At June 2008, an estimated 11.6 per cent of nursing homes were planning building work.
Quality, complaints and compliance
- During 2007-08 the Aged Care Standards and Accreditation Agency conducted 5,244 visits to homes, with 3,105 visits being unannounced. In this same period the Department undertook 3,127 visits to homes, of which 1,145 were unannounced.
- The Accreditation Agency identified 46 homes (1.6 per cent) that had some non-compliance in relation to the 44 accreditation standard outcomes.
- The Aged Care Complaints Investigation Scheme (CIS) referred 1,770 matters to the Accreditation Agency, 62 to Nurses' Registration Boards, 53 to the police; 33 to the Coroner; 27 to the Health Care Complaints Commission and 13 to the Medical Practitioners Board.
- Twenty-two percent of the referrals to the Accreditation Agency requested a support contact or a review audit of a nursing home.
- During 2007-2008, the Department of Health and Ageing applied sanctions against 14 providers, issuing 15 Notices of Decision to Impose Sanctions and issued 75 Notices of Non-Compliance.
- The CIS received 11,323 contacts between July 1, 2007 and June 30, 2008 of which 66 per cent were able to be investigated as these related to approved providers' responsibilities under the Aged Care Act 1997 (the Act).
- The most common issues reported to the CIS in order were: Health and Personal care (3,106 cases), physical environment (1,598 cases), consultation and communication (1,496 cases), personnel (1,255 cases) and 1,117 cases relating to alleged abuse.
Breaches under the Aged Care Act
- The CIS identified 930 breaches of an approved provider's responsibility.
- There were 214 Notices of Required Action issued by the CIS requiring providers to address a breach.
Of the remaining number of breaches, the matters were resolved through a negotiated outcome or through referral to another agency.
Of the 930 breaches identified:
- 36 per cent (333) were in Victoria;
- 25 per cent (231) were in NSW;
- 17 per cent (162) were in Queensland;
- 9 per cent (84) were in WA;
- 6 per cent (53) were in SA;
- 4 per cent (39) were in Tasmania;
- 2 per cent (17) were in ACT; and
- 1 per cent (11) was in NT.
Notices of Required Action (NRAs)
214 Notice of Required Actions were issued where approved providers were found to be in breach of the Act and had not taken action to rectify the breach:
- 40 per cent (86) of all NRAs were in Queensland;
- 22 per cent (47) were in NSW;
- 15 per cent (32) were in South Australia;
- 9 per cent (20) were in Victoria;
- 4 per cent (8) were in both Western Australia and Tasmania;
- 3 per cent (7) were in the Northern Territory; and
- 3 per cent (6) were in the Australian Capital Territory.
Alleged Reportable Assaults
There were 925 notifications of alleged reportable assaults.
- Of those 725 were recorded as alleged unreasonable use of force and 200 were alleged unlawful sexual contact:
NSW had 323 alleged reportable assaults,
275 were alleged serious physical assault,
48 were alleged sexual assault;
Queensland had 225 alleged reportable assaults
174 were alleged serious physical assault,
51 were alleged sexual assault;
Victoria had 224 alleged reportable assaults
152 were alleged serious physical assault,
72 were alleged sexual assault;
SA had 86 alleged reportable assaults
69 were alleged serious physical assault,
17 were alleged sexual assault;
WA had 33 alleged reportable assaults
27 were alleged serious physical assault,
6 were alleged sexual assault;
Tasmania had 28 alleged reportable assaults
23 were alleged serious physical assault,
5 were alleged sexual assault;
Australian Capital Territory had 5 alleged reportable assaults
4 were alleged serious physical assault,
1 was an alleged sexual assault; and
Northern Territory had 1 reportable assault, which was an alleged serious physical assault.
Police are responsible for determining whether charges should be laid. As this is a police matter, within the jurisdiction of each State and Territory, the CIS is unable to track if and when charges are laid.
For more information, contact Mrs Elliot's office on (02) 6277 7280
The data: 1 July 2007 - 30 June 2008
Table 1: Aged-care homes that failed some non-compliance over period of 1 July 2007 - 30 June 2008
* = Sanctioned nursing homes; PFP = Private-for-profit; Govt. = Government; Sanc. Date = Sanction/s Date; NFP/R = Not for Profit: Religious; NFP/CH = Not for Profit: Charitable; NFP/CB = Not for Profit: Community Based
State | Approved Provider | Prov. type | Stds. failed | Audit Date | Service Name | Sanctioned |
|---|---|---|---|---|---|---|
SA | Goel Nominees Pty Ltd | PFP | 1 | 06.08.07 | Abbingdon Private Nursing Home | |
TAS | Southern Cross Care (Tas) Inc | NFP/R | 6 | 26.11.07 | Ainslie House Hostel | |
TAS | Southern Cross Care (Tas) Inc | NFP/R | 6 | 26.11.07 | Ainslie Nursing Home | |
VIC | Allambi Elderly Peoples Home Inc. | NFP/CB | 21 | 28.05.07 | Allambi Elderly Peoples Home* | 19/10/07 |
VIC | Kwok Nominees Pty Ltd | PFP | 5 | 01.10.07 | Andrina Private Nursing Home | |
VIC | Derby Place Pty Ltd | PFP | 2 | 28.08.07 | Ardmillan Place | |
VIC | Expanding Horizons National Pty Ltd | PFP | 30 | 12.09.07 | Ashleigh Aged Care* | 16/9/07 |
VIC | Aged Care Services Three (Balmoral Grove) Pty Ltd | PFP | 10 | 03.03.08 | Balmoral Grove | |
NSW | Temahl (AUST) Pty Ltd | PFP | 13 | 21.04.08 | Bangalor Retreat | |
VIC | Glengail Pty Ltd | PFP | 2 | 20.05.08 | Bellrise Aged Care Facility | |
VIC | Saitta Pty Ltd | PFP | 26.09.07 | Belvedere Park Nursing Home* | 16/8/07 | |
NSW | Booroongen Djugun Aboriginal Corporation | NFP/CB | 9 | 30.03.08 | Booroongen Djugun Aboriginal Corporation | |
VIC | Vitality Care Commissioning Pty Ltd | PFP | 17 | 22.05.08 | Bridgewater Aged Care | |
QLD | Bundaleer Lodge Nursing Home Pty Ltd | PFP | 1 | 21.01.08 | Bundaleer Lodge Nursing Home | |
QLD | Queensland Rehabilitation Services Pty Ltd | PFP | 4 | 16.07.07 | Carindale Brook Innovative Care Centre | |
QLD | The Uniting Church in Australia Property Trust (Q) | NFP/R | 16 | 18.12.07 | Carramar Complex | |
VIC | Chaffey Aged Care | NFP/CH | 6 | 26.11.07 | Chaffey Aged Care | |
NSW | Clermont Nursing Home Pty Ltd | PFP | 4 | 26.02.08 | Clermont Nursing Home | |
VIC | St Arnaud Elderly Persons Hostel Inc | NFP/CB | 3 | 26.11.08 | Coates Hostel | |
VIC | Corpus Christi Community Greenvale Incorporated | NFP/CH | 13 | 04.07.07 | Corpus Christi Community | |
SA | St Basil's Homes for the Aged in South Australia (Vasileias) Inc | NFP/CH | 4 | 17.07.07 | Croydon Park Aged Care Facility | |
VIC | Caulfield Drive Pty Ltd | PFP | 14 | 20.08.07 | Dava Lodge Residential Aged Care Facility | |
WA | Western Australian Baptist Hospital & Homes Trust Inc | NFP/R | 2 | 03.12.07 | David Buttfield Centre | |
QLD | Aborigines and Islanders Alcohol Relief Services Ltd | NFP/CB | 3 | 11.03.08 | Dija Meta Aged & Disabled Hostel (Hartley Street) | |
VIC | B & E O'Connor Pty Ltd | PFP | 1 | 17.03.08 | Drysdale Grove | |
QLD | Bindaree Lodge Management Board Inc | NFP/CB | 17 | 26.11.07 | Edenvale | |
VIC | Edgarley Home Inc | NFP/CB | 10 | 19.06.08 | Edgarley Home (Edgarley Hostel) | |
QLD | Queensland Health | Govt. | 1 | 28.03.08 | Eventide Nursing Home Sandgate | |
QLD | Lollies Management Pty Ltd | PFP | 1 | 23.07.07 | Forest Lake Lodge | |
TAS | Glenview Home Inc | NFP/CH | 1 | 02.07.07 | Glenview Home | |
SA | Goel Nominees Pty Ltd | PFP | 21 | 09.07.07 | Gloucester Residential Care | |
WA | ACK Pty Ltd | PFP | 1 | 11.12.07 | Grandview Aged Care | |
QLD | Domain Aged Care NO. 2 | PFP | 4 | 30.06.08 | Greenfern Place | |
VIC | Parkwood Aged Care Services | PFP | 1 | 06.05.08 | Grossard Court | |
WA | Nindilingarri Cultural Health Services Inc | NFP/CB | 3 | 10.07.07 | Guwardi Ngadu Hostel | |
WA | Hamersley Nursing Home (WA) Pty Ltd | PFP | 1 | 25.09.07 | Hamersley Nursing Home | |
NT | Aboriginal Hostels Limited | NFP/CB | 15 | 11.10.07 | Hetti Perkins Home for the Aged (6982)* | 17/10/07 |
NT | Aboriginal Hostels Limited | NFP/CB | 15 | 11.10.07 | Hetti Perkins Home for the Aged (6992) | |
QLD | People Care Pty Ltd | PFP | 4 | 31.07.07 | Hibiscus House Nursing Home | |
QLD | The Baptist Union of Queensland | NFP/R | 9 | 28.08.07 | Hilltop Gardens Care Centre | |
VIC | Doutta Galla Aged Services Ltd | NFP/CH | 1 | 11.03.08 | Howard Kingham Lodge | |
SA | Montbello Pty Ltd | PFP | 11 | 25.06.07 | Hyde Park Aged Care* | 27/09/07 |
QLD | Lutheran Church of Australia - Queensland District | NFP/R | 9 | 12.06.08 | Immanuel Gardens Hostel | |
VIC | Retirement Care Australia (Inala) Pty Ltd | PFP | 6 | 31.08.07 | Inala Village Nursing Home | |
WA | Dale Cottages (Inc.) | NFP/CB | 27 | 30.10.07 | J E Murray Home | |
VIC | Johnson-Goodwin Memorial Homes | NFP/CB | 8 | 07.08.07 | Johnson-Goodwin Memorial Homes | |
QLD | Killarney & District Memorial Hospital Limited | NFP/CB | 8 | 08.01.08 | Kadimah Nursing Home | |
VIC | Aged Care Services One (Central Park) Pty Ltd | PFP | 5 | 03.07.07 | Kiverton Park Nursing Home | |
VIC | Edenhope & District Memorial Hospital | Govt. | 1 | 24.07.07 | Kowree Nursing Home Unit | |
QLD | Bynoe Community Advancement Co-Operative Society Ltd | NFP/CB | 18 | 13.09.07 | Kukatja Place | |
VIC | Latrobe Private Nursing Home Pty Ltd | PFP | 2 | 26.02.08 | Latrobe Private Nursing Home | |
QLD | Leichhardt Villa Inc | NFP/CB | 1 | 27.05.08 | Leichhardt Villa Inc Hostel | |
QLD | Killarney & District Memorial Hospital Limited | NFP/CB | 8 | 08.01.08 | Leslie Place Aged Persons Hostel | |
QLD | Lifestyle Care Providers Pty Ltd | PFP | n/a | n/a | Lifecare Goldcoast* | 21/07/07 |
SA | Central Northern Adelaide Health Service | Govt. | 26 | 10.12.07 | Makk And McLeay Nursing Home* | 14/12/07 |
NSW | Maranatha House | PFP | 1 | 29.04.08 | Maranatha House | |
QLD | Booringa Shire Council | Govt. | 13 | 10.06.08 | Maranoa Retirement Village | |
TAS | Masonic Peace Memorial Haven of Northern Tasmania Inc | NFP/CB | 3 | 16.07.07 | Masonic Peace Memorial Haven | |
TAS | Masonic Peace Memorial Haven of Northern Tasmania Inc | NFP/CB | 2 | 16.07.07 | Masonic Peacehaven Hostel | |
QLD | The Uniting Church in Australia Property Trust (Q) | NFP/R | 12 | 21.08.07 | Masters Lodge Hostel | |
QLD | Shownoff Pty Ltd | PFP | 8 | 06.11.07 | Mudgeeraba Lodge | |
QLD | Shownoff Pty Ltd | PFP | 25 | 01.11.07 | Mudgeeraba Nursing Centre* | 5/11/07 |
NSW | Principal Healthcare Finance No 3 Pty Limited | PFP | 14 | 14.01.08 | Murwillumbah Nursing Home | |
QLD | North Stradbroke Island Aboriginal & Islander Housing Co-Operative Society Limited | NFP/CB | 3 | 01.04.08 | Nareeba Moopi Moopi Pa Aged Care Hostel | |
WA | Principal Healthcare Finance No 3 Pty Limited | PFP | 28 | 09.11.07 | Narrogin Nursing Home | |
QLD | The Nazareth Lutheran Church of South Brisbane | NFP/R | 2 | 07.08.07 | Nazareth Residential Aged Care | |
QLD | Cherbourg Community Council | Govt. | 11 | 18.02.08 | Ny-Ku Byun* | 13/06/08 |
WA | Catholic Homes Incorporated | NFP/R | 3 | 24.07.07 | Ocean Star Aged Care | |
SA | L P Rositano & M Rositano & R M Rositano and S P Rositano | PFP | 18 | 17.12.07 | Para Hills Private Nursing Home | |
SA | Retirement Care Australia (Parklyn) Pty Ltd | PFP | 2 | 06.06.08 | Parklyn Senior Citizens Residence | |
VIC | Melbourne Health | Govt. | 6 | 18.11.07 | Parkville Hostel | |
NSW | Catholic Healthcare Holdings Limited | NFP/CH | 10 | 28.11.07 | Paulian Villa | |
QLD | Regis Group Pty Ltd | PFP | 11 | 02.01.08 | Regis Caboolture | |
SA | Renmark Paringa District Hospital Inc | Govt. | 19 | 10.09.07 | Renmark & Paringa District Hospital Hostel | |
SA | Renmark Paringa District Hospital Inc | Govt. | 18 | 10.09.07 | Renmark Nursing Home | |
SA | Fairlux Pty Ltd | PFP | 19 | 08.10.07 | Ridge Park Health Care Centre* | 12/10/07 |
SA | Greek Orthodox Community of SA Inc | NFP/R | 11 | 03.03.08 | Ridleyton Greek Home for the Aged* | 29/02/08 |
SA | Maketa Pty Ltd | PFP | 1 | 30.01.08 | Rose Court Aged Care Facility | |
QLD | Joronco Pty Ltd | PFP | 4 | 06.08.07 | Rosevale Court | |
SA | The Society of St Hilarion Inc | NFP/R | 7 | 06.11.07 | Saint Hilarion Aged Care Lockleys* | 13/11/07 |
SA | Arcanola Pty Ltd | PFP | 16 | 02.06.08 | Salisbury Gardens Aged Care Service | |
QLD | Southern Cross Care (QLD) Inc | NFP/R | 2 | 11.03.08 | Southern Cross Care Facility Caloundra | |
VIC | St Benedicts Private Nursing Home Pty Ltd | PFP | 4 | 25.03.08 | St Benedict's Private Nursing Home | |
SA | Anglicare SA Inc | NFP/R | 4 | 11.02.08 | St Laurence's Court Nursing Home | |
SA | Strathalbyn and District Health Service | Govt. | 6 | 29.10.07 | Strathalbyn & District Aged Care Facility | |
WA | ACK Pty Ltd | PFP | 22 | 07.08.07 | Tanby Hall | |
NSW | Christadelphian Homes | NFP/R | 8 | 12.04.08 | The Bay Nursing Home | |
VIC | Western Residential Aged Care Pty Ltd | PFP | 7 | 16.10.07 | The Belmont Residential Aged Care | |
SA | Jakudo Pty Ltd | PFP | 2 | 27.08.07 | The Kensington Residential Care Facility* | 2/07/07 |
QLD | Tricare (Annerley) Pty Ltd | PFP | 11 | 25.01.08 | TriCare Annerley Nursing Centre | |
VIC | Java Dale Pty Ltd | PFP | 8 | 15.02.08 | Trinity Garden Aged Care (formerly Western Private Nursing Home) | |
TAS | OneCare Limited | NFP/CH | 7 | 01.10.07 | Umina Park Home For The Aged | |
TAS | OneCare Limited | NFP/CH | 6 | 01.10.07 | Umina Park Hostel | |
VIC | Aged Care Services Six (Mirridong) Pty Ltd | PFP | 1 | 23.07.07 | Viewhills Manor | |
VIC | Warley Hospital Inc | NFP/CB | 3 | 15.11.07 | Warley Nursing Home | |
QLD | Queensland Health | Govt. | 1 | 02.10.07 | Waroona Multipurpose Centre | |
QLD | Churches of Christ in Queensland | NFP/R | 12 | 11.03.08 | Warrawee Retirement Village | |
QLD | Warrina Innisfail | NFP/CB | 10 | 27.11.07 | Warrina Innisfail Hostel | |
QLD | Warrina Innisfail | NFP/CB | 12 | 27.11.07 | Warrina Innisfail Nursing Home (Multi-Cultural) | |
VIC | Melbourne Health | Govt. | 5 | 13.05.08 | Weighbridge Residential Care Facility | |
NSW | William Cape Gardens Pty Limited | PFP | 3 | 05.03.08 | William Cape Gardens | |
SA | Vijon Holding Pty Ltd | PFP | 16 | 14.04.08 | Winchester Residential Care | |
QLD | Seventh - day Adventist Aged Care (South Queensland) Ltd | NFP/CH | 11 | 29.05.08 | Wisteria Lodge | |
QLD | Wongaburra Society | NFP/CB | 13 | 15.05.08 | Wongaburra Garden Settlement Hostel | |
QLD | Wongaburra Society | NFP/CB | 11 | 15.05.08 | Wongaburra Nursing Home | |
NSW | Lutheran Aged Care Albury Inc | NFP/CH | 1 | 13.05.08 | Yallaroo | |
QLD | Churches of Christ in Queensland | NFP/R | 1 | 03.07.07 | Yapunyah Lodge Hostel | |
QLD | Queensland Health | Govt. | 21 | 16.06.08 | Yaralla Place* | 20/06/08 |
The information in this table is based on information that we have been able to access published on-line (at various intervals) by the Aged Care Standards and Accreditation Agency (ACSAA) and the Department of Health and Ageing (DHA). The current limited system of late release and early removal of adverse reports from the Aged Care Standards and Accreditation Agency website is unsatisfactory. Based on the limited information that is publicly available, the data may not be contemporaneous and these findings are tentative.
Lack of transparency: An unfulfilled promise
The government had promised greater transparency but there is little evidence of this in the aged care sector - particularly from a consumer perspective. If the Accreditation Agency and Government departments are doing their job then they should be collating the material and graphing it from a consumer's perspective. There must be far more involvement from communities and much more consumer input into these processes.
The current limited system of late release and early removal of adverse reports from the Aged Care Standards and Accreditation Agency website, and information provided by the Department of Health and Ageing, is unsatisfactory.
General comments
The current limited system of late release, and early removal of adverse reports, from the Aged Care Standards and Accreditation Agency website is unsatisfactory. Consumers are entitled to disclosure of past, as well as present, oversight (accreditation) reports. Recurrent offenders are of most concern. The Accreditation Agency should openly publish all reports (the old website accommodated historical reports prior to 2005 but has not since then). The community should be able to see what the company or provider is capable of when no one is watching - not just when they have been given time to prepare and not after they had responded to an adverse finding in order to stay in business.
One of the most remarkable and inexplicable things about the accreditation process is the total absence of any meaningful data from the nursing homes.
The agency does not expect the facility to disclose its incidence of pressure sores, contractures, weight loss and dehydration, complaints, incident reports, improvement logs, etc, nor do they verify the accuracy of data provided and report on it.
Consumers should examine the track record of the owner in his/her other homes. It is the owner who allocates funding and dictates policy. Consumers should visit the home unannounced and be given access, preferably during a meal time, to see the quality of food and whether there are staff helping residents to eat. A pervasive smell of urine or faeces is a warning. Facilities for physical exercise and mental stimulation are important.
Relatives are often unaware of the key relationship between bad nursing and the deteriorating condition of the elderly resident. Weight loss, dehydration, pressure sores, contractures, being bedridden, and mental deterioration may be accepted as due to ageing rather than to bad nursing, excess sedation, insufficient exercise and a lack of mental stimulation.
Insufficient and untrained staff is a key problem. Prospective residents and their families should obtain staffing information and have the knowledge to assess staffing ratios. This is the sort of information you require when you are evaluating a nursing home.
Glossary
- Accreditation: Accreditation is the evaluation process which aged care homes must undergo to continue receiving residential care subsidies from the Australian Government.
- Aged Care Standards and Accreditation Agency: (Changed name to the Australian Aged Care Quality Agency) is responsible for the accreditation of aged-care facilities, in line with the current federal government policy of self-regulation by industry.
- Accreditation Standards: Homes are assessed against four Accreditation Standards: Management Systems, Staffing and Organisational Development; Health and Personal Care; Resident Lifestyle and Physical Environment and Safe Systems. Each standard is divided into a number of Expected Outcomes. There are 44 Expected Outcomes across the four Accreditation Standards.
- Approved Provider: A person or organisation approved under Part 2.1 of the Aged Care Act to be a provider of care for the purpose of payment of subsidy (A provider approved since the commencement of the Act must be a corporation.)
- Sanction: A sanction (or multiple sanctions, depending upon the level of non-compliance/s) is a penalty imposed by the Department of Health and Ageing on operators of residential aged care facilities in cases of what they deem to be serious non-compliance with the provisions of the Aged Care Act 1997.
- Notices of Non-compliance (NNCs): Notices of Non-Compliance are issued by the Department when an approved provider has not complied with its responsibilities in providing required care and services but where this has not caused an immediate and severe risk to care recipients' health, safety or well being. The Notice issued to the provider makes clear what problems need to be addressed and by when. The provider is expected to meet with care recipients, tell them about the identified problems and explain what it will be doing to fix them.